
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Altered Metabolic Phenotypes and Hypothalamic Neuronal Activity Triggered by Sodium-Glucose Cotransporter 2 Inhibition (Diabetes Metab J 2023;47:784-95)
- Ho Gyun Lee, Il Hyeon Jung, Byong Seo Park, Hye Rim Yang, Kwang Kon Kim, Thai Hien Tu, Jung-Yong Yeh, Sewon Lee, Sunggu Yang, Byung Ju Lee, Jae Geun Kim, Il Seong Nam-Goong
- Diabetes Metab J. 2024;48(1):159-160. Published online January 29, 2024
- DOI: https://doi.org/10.4093/dmj.2022.0458
- 660 View
- 93 Download
- Basic Research
- Altered Metabolic Phenotypes and Hypothalamic Neuronal Activity Triggered by Sodium-Glucose Cotransporter 2 Inhibition
- Ho Gyun Lee, Il Hyeon Jung, Byong Seo Park, Hye Rim Yang, Kwang Kon Kim, Thai Hien Tu, Jung-Yong Yeh, Sewon Lee, Sunggu Yang, Byung Ju Lee, Jae Geun Kim, Il Seong Nam-Goong
- Diabetes Metab J. 2023;47(6):784-795. Published online August 23, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0261
- 1,432 View
- 149 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
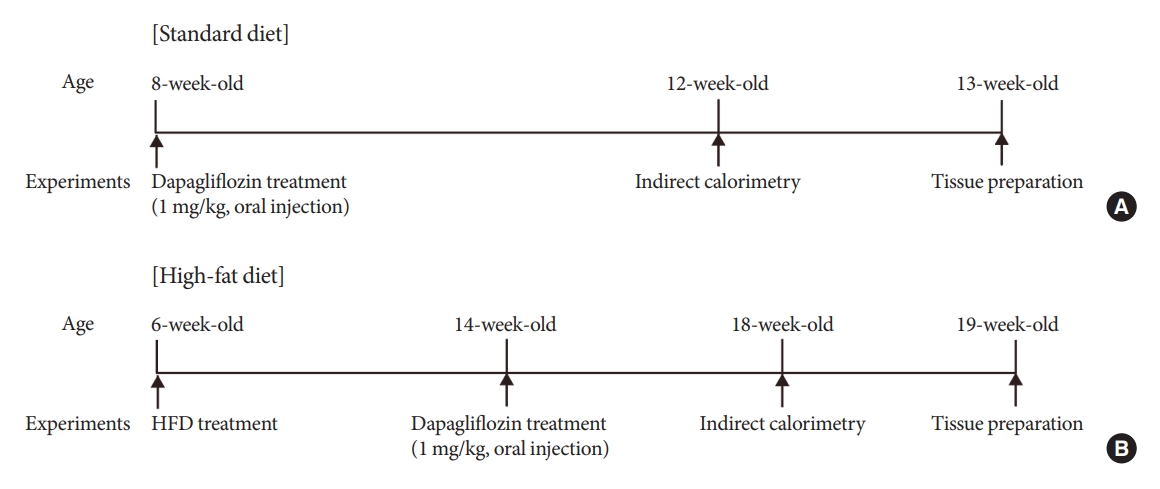
Sodium-glucose cotransporter 2 (SGLT-2) inhibitors are currently used to treat patients with diabetes. Previous studies have demonstrated that treatment with SGLT-2 inhibitors is accompanied by altered metabolic phenotypes. However, it has not been investigated whether the hypothalamic circuit participates in the development of the compensatory metabolic phenotypes triggered by the treatment with SGLT-2 inhibitors.
Methods
Mice were fed a standard diet or high-fat diet and treated with dapagliflozin, an SGLT-2 inhibitor. Food intake and energy expenditure were observed using indirect calorimetry system. The activity of hypothalamic neurons in response to dapagliflozin treatment was evaluated by immunohistochemistry with c-Fos antibody. Quantitative real-time polymerase chain reaction was performed to determine gene expression patterns in the hypothalamus of dapagliflozin-treated mice.
Results
Dapagliflozin-treated mice displayed enhanced food intake and reduced energy expenditure. Altered neuronal activities were observed in multiple hypothalamic nuclei in association with appetite regulation. Additionally, we found elevated immunosignals of agouti-related peptide neurons in the paraventricular nucleus of the hypothalamus.
Conclusion
This study suggests the functional involvement of the hypothalamus in the development of the compensatory metabolic phenotypes induced by SGLT-2 inhibitor treatment. -
Citations
Citations to this article as recorded by- Altered Metabolic Phenotypes and Hypothalamic Neuronal Activity Triggered by Sodium-Glucose Cotransporter 2 Inhibition (Diabetes Metab J 2023;47:784-95)
Jae Hyun Bae
Diabetes & Metabolism Journal.2024; 48(1): 157. CrossRef - Altered Metabolic Phenotypes and Hypothalamic Neuronal Activity Triggered by Sodium-Glucose Cotransporter 2 Inhibition (Diabetes Metab J 2023;47:784-95)
Ho Gyun Lee, Il Hyeon Jung, Byong Seo Park, Hye Rim Yang, Kwang Kon Kim, Thai Hien Tu, Jung-Yong Yeh, Sewon Lee, Sunggu Yang, Byung Ju Lee, Jae Geun Kim, Il Seong Nam-Goong
Diabetes & Metabolism Journal.2024; 48(1): 159. CrossRef
- Altered Metabolic Phenotypes and Hypothalamic Neuronal Activity Triggered by Sodium-Glucose Cotransporter 2 Inhibition (Diabetes Metab J 2023;47:784-95)
- Effects of Rosiglitazone on Inflammation in Otsuka Long-Evans Tokushima Fatty Rats
- Jin Woo Lee, Il Seong Nam-Goong, Jae Geun Kim, Chang Ho Yun, Se Jin Kim, Jung Il Choi, Young IL Kim, Eun Sook Kim
- Korean Diabetes J. 2010;34(3):191-199. Published online June 30, 2010
- DOI: https://doi.org/10.4093/kdj.2010.34.3.191
- 4,534 View
- 25 Download
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Inflammation plays a role in the response to metabolic stress in type 2 diabetes. However, the effects of rosiglitazone on inflammation of skeletal muscle have not been fully examined in type 2 diabetes.
Methods We investigated the effects of the insulin-sensitizing anti-diabetic agent, rosiglitazone, on the progression of skeletal muscle inflammation in Otsuka Long-Evans Tokushima Fatty (OLETF) type 2 diabetic rats. We examined the expression of serologic markers (serum glucose, insulin and free fatty acid) and inflammatory cytokines (tumor-necrosis factor-α, interleukin [IL]-1β and IL-6) in OLETF rats from early to advanced diabetic stage (from 28 to 40 weeks of age).
Results Serum glucose and insulin concentrations were significantly decreased in rosiglitazone-treated OLETF rats compared to untreated OLETF rats. Rosiglitazone treatment significantly decreased the concentrations of serum inflammatory cytokines from 28 to 40 weeks of age. The mRNA expression of various cytokines in skeletal muscle was reduced in rosiglitazone-treated OLETF rats compared with untreated OLETF rats. Furthermore, rosiglitazone treatment resulted in the downregulation of ERK1/2 phosphorylation and NF-κB expression in the skeletal muscle of OLETF rats.
Conclusion These results suggest that rosiglitazone may improve insulin sensitivity with its anti-inflammatory effects on skeletal muscle.
-
Citations
Citations to this article as recorded by- Rosiglitazone Elicits an Adiponectin-Mediated Insulin-Sensitizing Action at the Adipose Tissue-Liver Axis in Otsuka Long-Evans Tokushima Fatty Rats
Jia Li, Yao-Ming Xue, Bo Zhu, Yong-Hua Pan, Yan Zhang, Chunxia Wang, Yuhao Li
Journal of Diabetes Research.2018; 2018: 1. CrossRef - Sirt1 and Sirt6 Mediate Beneficial Effects of Rosiglitazone on Hepatic Lipid Accumulation
Soo Jin Yang, Jung Mook Choi, Eugene Chang, Sung Woo Park, Cheol-Young Park, Aimin Xu
PLoS ONE.2014; 9(8): e105456. CrossRef - Beneficial effects of co-enzyme Q10 and rosiglitazone in fructose-induced metabolic syndrome in rats
Suzan M. Mansour, Hala F. Zaki, Ezz-El-Din S. El-Denshary
Bulletin of Faculty of Pharmacy, Cairo University.2013; 51(1): 13. CrossRef - Chromium Picolinate and Rosiglitazone Improve Biochemical Derangement in a Rat Model of Insulin Resistance: Role of TNF-a and Leptin
Suzan M. Mansour, Hala F. Zaki, Ezz-El-Din El-Denshar
Pharmacologia.2013; 4(3): 186. CrossRef - Angiotensin Receptor Blockade Increases Pancreatic Insulin Secretion and Decreases Glucose Intolerance during Glucose Supplementation in a Model of Metabolic Syndrome
Ruben Rodriguez, Jose A. Viscarra, Jacqueline N. Minas, Daisuke Nakano, Akira Nishiyama, Rudy M. Ortiz
Endocrinology.2012; 153(4): 1684. CrossRef - Rodent Models for Metabolic Syndrome Research
Sunil K. Panchal, Lindsay Brown
Journal of Biomedicine and Biotechnology.2011; 2011: 1. CrossRef - Letter: Effects of Rosiglitazone on Inflammation in Otsuka Long-Evans Tokushima Fatty Rats (Korean Diabetes J 2010;34:191-9)
Soo Jin Yang, Cheol-Young Park
Korean Diabetes Journal.2010; 34(4): 261. CrossRef
- Rosiglitazone Elicits an Adiponectin-Mediated Insulin-Sensitizing Action at the Adipose Tissue-Liver Axis in Otsuka Long-Evans Tokushima Fatty Rats
- The Role of Hypothalamic FoxO1 on Hyperphagia in Streptozotocin-Induced Diabetic Mice.
- Il Seong Nam-Goong, Jae Geun Kim, Se Jin Kim, Seong Jae Hur, Jin Woo Lee, Eun Sook Kim, Chang Ho Yun, Byung Ju Lee, Young Il Kim
- Korean Diabetes J. 2009;33(5):375-381. Published online October 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.5.375
- 1,950 View
- 22 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Streptozotocin-induced diabetic animals are characterized by hyperphagia due to deficiencies of insulin and leptin. Forkhead box-containing protein of the O subfamily-1 (FoxO1) regulates energy homeostasis by regulating energy expenditure and food intake as well as mediating insulin and leptin signals in the hypothalamus. To identify the mediator of diabetic hyperphagia, we examined the effects of insulin or leptin on hypothalamic FoxO1 expression in a diabetic animal model. METHODS: Diabetes was induced in mice (C57BL/6) by intraperitoneal administration of streptozotocin (200 mg/kg). Stainless steel cannula was implanted into the lateral ventricle of the brain in each mouse. After three weeks, the mice were administered saline, insulin or leptin via intracerebroventricular (ICV) route. The medial hypothalamus was isolated to evaluate the mRNA expressions of FoxO1 and neuropeptides. RESULTS: Streptozotocin-induced diabetic mice exhibited significant elevations of blood glucose and food intake and significantly low levels of serum insulin and leptin. The levels of hypothalamic FoxO1 mRNA were significantly increased in diabetic mice. The hypothalamic expression of neuropeptide Y (NPY) mRNA was increased, but the expression of preproopiomelanocortin (POMC) mRNA was decreased in diabetic mice. ICV administration of insulin or leptin attenuated the upregulation of hypothalamic FoxO1 mRNA, and resulted in downregulation of NPY mRNA and upregulation of POMC mRNA in diabetic mice. CONCLUSION: We observed that the expression of hypothalamic FoxO1 mRNA was increased in streptozotocin-induced diabetic mice, and that it was significantly attenuated by central administration of insulin or leptin. These results suggest that hypothalamic FoxO1 is the direct mediator of diabetic hyperphagia.

 KDA
KDA
 First
First Prev
Prev





